Measuring Medication Adherence: Exploring Issues and Better Solutions
Written by James Lee
Director, Innovative Solutions - Medication Adherence
Ensuring medication adherence is a critical aspect of patient care, directly influencing treatment outcomes and overall health. However, accurately measuring adherence has been a persistent challenge in the pharmacy and healthcare industry.
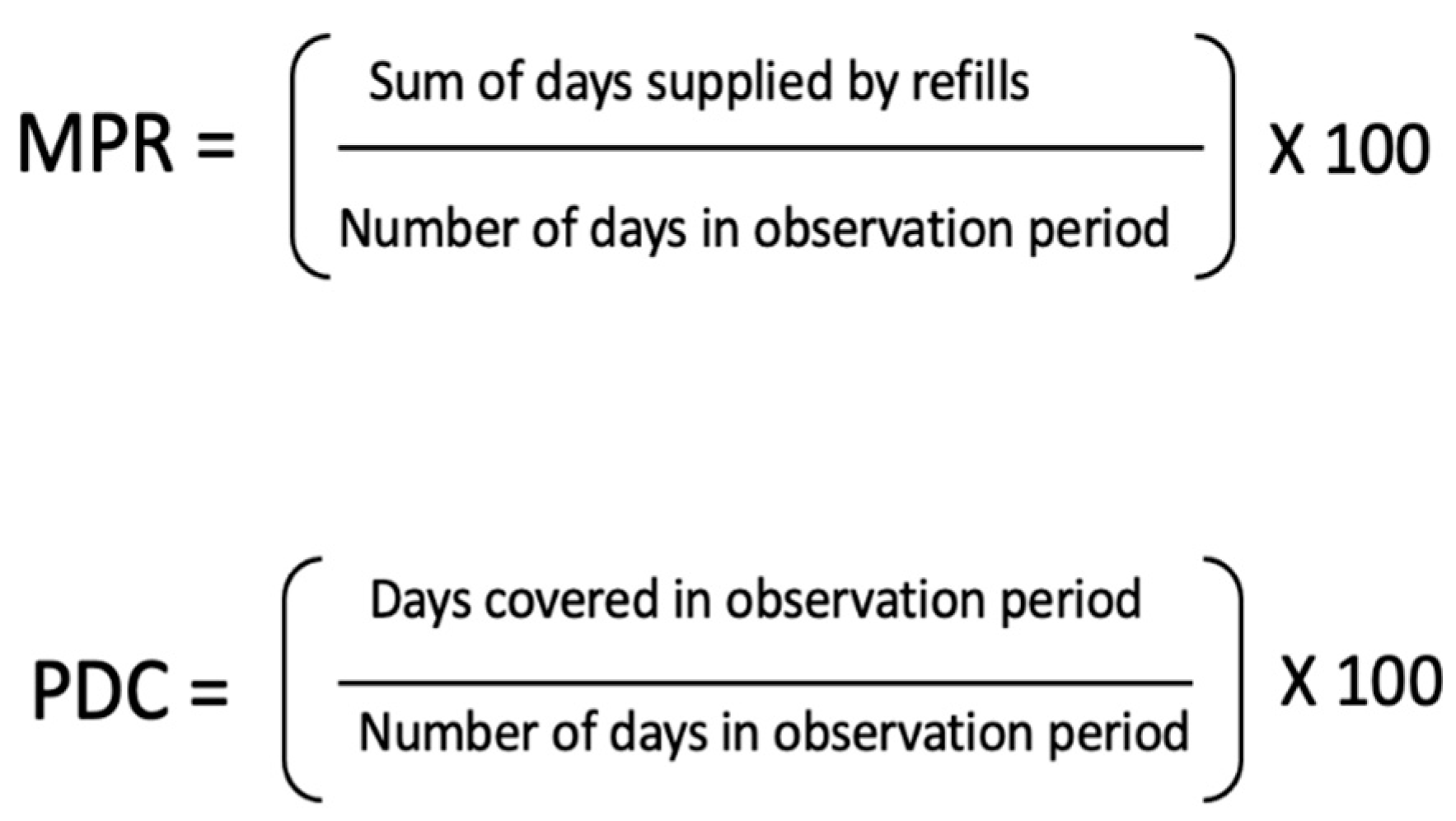
The traditional methods of measurement, including the Medication Possession Ratio (MPR) and Proportion of Days Covered (PDC) have limitations. These methods fail to provide a comprehensive understanding of true medication adherence. In this article, I will delve into the shortcomings of current measurements and explore innovative solutions that can improve the way we evaluate adherence.
The Limitations of MPR and PDC
The most accurate way to measure medication adherence is via pharmacokinetic modelling, a direct measurement that looks at drug concentrations in a patient’s blood or urine. Although this is not a feasible way for clinicians or pharmacists to measure patient adherence more broadly and regularly. With this, the indirect MPR and PDC measurements have long been relied upon as indicators of medication adherence.
Source: https://www.mdpi.com/2226-4787/10/5/124It is essential to recognize, however, that these metrics primarily measure refill compliance, rather than actual medication adherence. The MPR is the sum of the days' supply for all fills of a given drug over a particular time period, divided by the number of days in that time period. The PDC is the number of days “covered” with prescribed medication over a period of time, divided by the number of days in that time period.
While they both offer some insights into whether patients have received their medications as prescribed, they do not reflect whether patients are actively taking them.
One of the most critical flaws in these measurements is that they often overestimate adherence rates. For example, we ran trials with specialty pharmacy patients that revealed significant discrepancies between PDC and adherence scores.
These scores are measured as doses taken compared to doses received, expressed as a percentage. Despite a high PDC of 0.92 or 92%, the adherence score for patients in the trial was only 0.65 or 65%. Such disparities emphasize the need for more accurate methods to assess medication adherence.
In the United States, star ratings measure pharmacy quality, with higher ratings indicating better adherence rates. However, the reliance on flawed data such as inflated PDC scores, undermines the accuracy of these ratings. This not only misrepresents pharmacy performance but also impedes the identification of patients in need of targeted interventions to improve adherence.
Evolution of Adherence Measurement
To address the limitations of traditional adherence measurements, a continuum of solutions is now available – from more basic calendarized packaging to technology-enabled medication adherence packaging solutions.
These advancements enable a more accurate assessment of medication adherence by measuring medication doses removed from packaging compared to doses received. While this does not confirm medication intake definitively––only measuring blood or urine concentrations can achieve this— it has been shown to be highly accurate in measuring medication adherence in several studies[1].
1. Blister packs: Blister packs are a type of calendarized packaging that pharmacies prepare for patients. Medication doses are sealed in compartments labeled by the time of day and/or day of the week they should be taken. These packs provide an effective solution since patients can return used packaging to the pharmacy. Pharmacists can then see whether all medications in the pack have been taken, or whether doses were missed. This approach fosters counselling and conversations with patients, promoting a better understanding of their medication intake and potential adherence challenges.
2. NFC (Near Field Communication)-enabled blister packaging: NFC technology empowers patients to log medication adherence in real time. By tapping their phone to an NFC tag on a blister pack each time they take a dose, patients can confirm and record their adherence data in the cloud. Our trials with Jones Healthcare’s CpaX™ NFC Adherence Platform have shown promising results, with a 12% improvement in average adherence scores and a 15% reduction in missed doses over a nine-week period.
3. Electronic Adherence Card (EAC): EAC systems achieve real-time adherence tracking. Each time a patient removes medication from a pack, the pack sends a signal to a cloud-based portal for tracking. This approach offers accurate, real-time insights into medication intake, facilitating timely interventions for patients at risk of non-adherence. Trials of our CpaX EAC Platform by the University of Waterloo confirm positive impacts of this packaging on older adults with chronic conditions.
By monitoring patient behaviour through technology-enabled platforms, pharmacies can focus on targeted interventions for patients with low adherence while still keeping high-performance patients under surveillance. This proactive approach minimizes the need for contacting all patients to determine adherence, allowing for more efficient use of resources. Technology-enabled blister packs can also deliver reminders via text message or phone call to patients and/or caregivers that a medication should be taken.
Overall, accurately measuring medication adherence is a crucial aspect of improving patient health outcomes and enhancing pharmacy performance. The limitations of traditional measurements, such as MPR and PDC, have prompted the exploration of innovative solutions utilizing technology.
Standard blister packs, NFC blister packs, and EAC systems offer improved methods for evaluating adherence based on actual doses taken as a function doses received. Embracing these advancements, such as the CpaX™ Adherence Platform, can improve adherence measurement, leading to better patient care and outcomes in the pharmacy setting.
[1] https://www.hindawi.com/journals/bmri/2015/217047About the Author James Lee
James is the Director of the Innovation Solutions Group at Jones Healthcare, where he is responsible for a team developing new packaging products for our customers. In his role, James focuses on new packaging technologies for tomorrow and their potential impact and outcomes for patients, consumers, pharmacists, and brand owners.
Since 2013, James has been focused on developing connected packaging solutions, particularly in their capacity to improve patient medication adherence. This long standing commitment has given him a deeper understanding of the factors associated with non-adherence.
Backed by 25 years of experience in printing and packaging using multiple production processes, he approaches solutions that are scalable and manufacturable in our current environments.